The Therapists 5 R's of Rehab
This is a concept/methodology we have used at Cor-Kinetic for quite a while and forms a loose framework of our considerations involved in the rehabilitation process. It is by no means an exhaustive or definitive list of all the considerations that may need to be considered however!
These considerations are taking into account not just the physiological or anatomical but also the CNS and beyond that the ‘human’ interpretation of this process that can sometimes be a little forgotten when focusing on the 'problem' component such as a tendon or area such as the lower back.
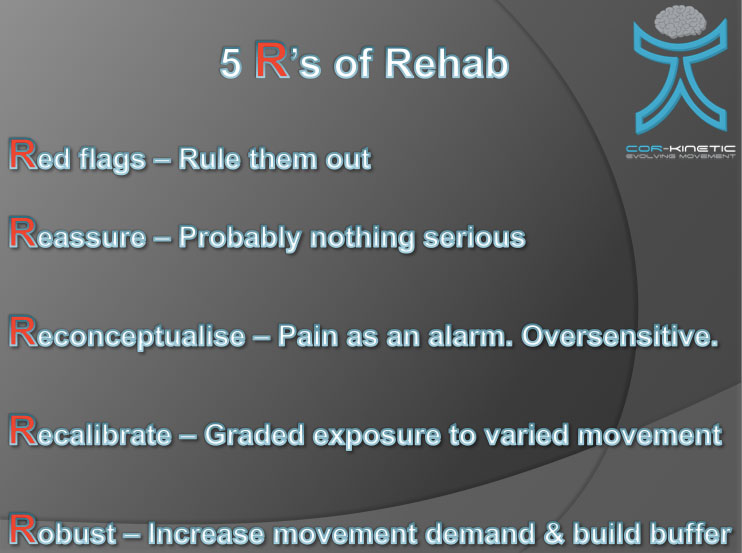
Red flags
It is always important to rule out any potential red flags that maybe present. Those qualified to do so will know what to do, those who aren’t, such as exercise professionals involved in rehab, should seek the advice of someone who is!!
It is always important to know when to refer out to another skill set when things outside of your skill set occur. If you are unsure then refer. Even the best laid rehab plans can encounter situations that need specialist help when complications arise outside of the normal course of events.
Reassure
The power of reassurance cannot be overstated in my opinion. Worry is another stressor to add to the stressor of being in pain. In fact it may turn into a bit of a stress loop.
Someone could be stressed out about being in pain and they may also be stressed about the reasons why they are in pain, the associated loss of function and the implications for their future.
Possible thoughts and questions:
Will the pain go away?
Why do I have this pain?
Is it here forever?
Why can no one help me?
Am I broken?
Now the pain gets worse because of the added stress and worry.
The loop is complete - the pain stresses people out and in turn the stress turns up the pain experience.
This may transition into hyper vigilance with every little twinge being interpreted as a little more threatening than before or potentially avoiding specific movements or activities that hurt contributing to beliefs about their fragility causing fear avoidance behaviours.
Maybe this has also been influenced by what they have read on the internet (Dr Google!) or have been told by their physio/chiro/osteo/trainer. People can pick up negative beliefs about their bad mechanics, weaknesses and MRI findings that have been related to them as "the crumbling spine of an 80 year old" that are pretty unhelpful and influence their perceptions of their current state and also their possible future state and capabilities.
In this paper *Click Here* even the word instability, used by so many in relation to back pain, maybe construed as:
“If they get you back to working order the back is unstable because the least little thing can actually throw it off again”
“Something's a bit loose ... It's liable to pop out”
So if you are an advocate of a more conservative approach, which many pain situations benefit from greatly it would seem, and the serious stuff has been ruled out then a little reassurance may go a long way to helping break the stress cycle.
The interpretation of an experience can have massive implications on the outcome. The placebo effect is very real in a chemical sense and can actually be reduced by drugs that block the natural opoids we produce. We have both pain reduction and pain enhancement processes in our pain systems.
If you are aware of this then you maybe able to frame your interaction to influence these systems positively and also understand what may influence them negatively.
Getting people on side with considered explanations in language they can relate to maybe just the ticket. If the likely hood is that they are not crippled for life and will be able to play with their kids again or do their shoelaces up without pain then let them know.
It is completely ethical in my opinion to try to maximize the parts of an experience that may contribute to it being more successful and help the pain reduction system kick in. Hoping for a placebo effect or using something that has be proven to be hit or miss and potential successes being attributed to the placebo effect maybe less ethical.
Reassurance, caring, compassion, understanding and empathy are all things that may contribute to a more successful outcome. Considering that they are influencing factors and maximizing their effect is considering the human rather than just the body part, muscle or the tendon.
Unfortunately the bit that makes us human is also difficult to quantify and is a little intangible. We maybe able to get pretty pictures of the parts of the brain that light up with different experiences but this still does not give us insight into conscious or subconscious processes that are occurring to form beliefs. We cannot always translate it into figures, tables and charts.
Seeing a ‘guru’ may have more to do with your beliefs in their magical powers rather than what they actually do or the methods they employ. Equally having a negative perception of something may contribute to its failure.
I really do not like needles; acupuncture therefore makes me stiff and tense and may negate or minimize the mechanism or placebo that could make it successful for me.
If we can generate a different perception and prediction of what the future may hold and start to increase someone’s internal locus of control it could benefit the rest of what you choose to do and ultimately the outcome achieved.
Reconceptualise
The rise of a better understanding of the science behind pain has been revolutionary for those in healthcare and physical fitness. Where the next quantum leap may come is transitioning this understanding to the people who are actually experiencing the pain!
Seeing pain as not just a reflection of the state of the tissue maybe extremely helpful for the chronic back pain sufferer in their 20’s who’s perception of their back is of an 80 year old with no sign of it getting and better or younger.
Explaining that hurt does not always equal harm may go a long way. There are some great examples when pain far outweighs the actual damage that has occurred.
Think getting a paper cut, an ice cream headache or even burning your finger. All of these events generate significant pain but with minimal damage that only take a little time to heal.
This is a great paper form Lorimer Moseley on reconceptualisng pain. *Click Here*
Let people know that essentially pain is a good thing. It stops us from burning ourselves for example or jumping off buildings and works as an alarm system to let us know that something is wrong. It has evolved over millions of years to be a powerful and subconscious protective mechanism involving our movement and sensations.
People who feel no pain, called 'Congenital Insensitivity to Pain' or CIP, tend to have a low life expectancy. Essentially pain is vital for survival.
Even your ankle hurting and swelling after you rolled it is a good thing. The pain stops you from putting more load through the tissue and the inflammation is working to help the healing process. It is a helpful adaptation to protect an injured body part.
Sometimes it becomes maladaptive or unhelpful. The tissue has healed but the protective alarm system still remains. No-one has come and switched it off. The default setting is actually too sensitive for the current state of the tissue.
It is a bit like the car alarm that keeps going off all night with just the slightest gust of wind. When you bend over you may trigger that really sensitive alarm system that is there to help but may need to be recalibrated a touch.
The ‘pain is in the brain’ line to reconceptualise may not work for all. The implication could be that there is something else wrong upstairs either physical or mental health. Instead it may be good to explain pain as changeable, that pain is not just a consistent signal that reflects tissue state and can be influenced by other factors.
Is pain a little like a stereo system? We have a CD player that sends its signal to the amplifier. The amplifier can then turn it up or down essentially modifying the signal. Sometimes we are feeling quiet and reflective and have the volume set lower. Sometimes we are angry and frustrated and turn it up full blast.
The signal from the CD player remains the same but the way we control the volume maybe dependent on our emotions, mood & current stresses. If you have seen ‘This is spinal tap’ you know what I mean when I say sometimes it gets turned up to 11!
Imagine you wake up after a great night’s sleep and stub your toe. You may brush it off and not give it another moments thought. Do the same after a long and stressful day and your response may be a little different even though essentially the act was the same.
Sport is a great example of when stressors can make us go a bit haywire. The pressures of winning or fear of losing can severely mess up the well-honed skills of the sports man. Just look at England's penalty kick record in major championships!
Recalibrate
So if the protective mechanisms have become too sensitive then someone needs come along and help them recalibrate a bit. Often people can be unaware of a change in their default settings. The sensitivity level becomes their normal. That could be the sensitivity in terms of sensations such as tightness or pain and motor responses that reduce range of motion.
Muscles going into spasm would be an extreme motor response to protect. Someone may experience this when they move to fast or pick something up to heavy and their back or neck ‘locks’.
We are often unaware of many of our behaviours until they are pointed out to us. Anger responses are normal for those with anger management issues. Often they are unaware of the default response of anger or how they can change it until they seek an outside perspective.
Just like Pavlov’s dog we can become conditioned to associate events. Instead of anticipating food we may anticipate pain and therefore create behaviors to protect against the impending problem. A subconscious stiffening of a joint before movement may form part of a behavior associated with an ongoing protective response.
The actual movement could pose very little ‘threat’ to the tissue but be perceived as having a much higher level of ‘threat’ based on previous experience of injury and pain. The alarm system may have been turned up to 11 and no one has come and turned it down. After a while we may get conditioned to this. We develop pain memories and then associated predictions of harm.
Helping recalibrate could be as simple as reducing some of these anticipatory responses. Someone with chronic shoulder pain may elevate their shoulder before moving it, contracting the traps and disrupting the smooth movement and normal range of the anatomy. You may see holding of the breath or grimacing.
Just highlighting this behavior and asking for relaxation prior to movement may change the mechanics sequence entirely and perhaps therefore the outcome. It could be far more a defense of the human than a defect of the anatomy or mechanics.
It is impossible to separate these things in my opinion, the human being the product of a number of complex systems interacting.
The problem may have nothing to do with the anatomy at all but instead how we subconscious perceive the state of the tissue. You could replace shoulder flexion with lumbar flexion or ankle inversion. In fact anywhere people may get recurrent problems.
My personal perspective, whatever that is worth and tainted by my personal bias, is that our motor responses may be a reflection of and help maintain our perceptions towards areas of our body. It is hard to know what is right and wrong so changing the current behavior and increasing the capacity and toleration of movement seems to be a pragmatic way to go.
The decrease in the variability of movement of those in and post pain is well documented. So if we want to assess and change this then a variety of movement tasks at different intensities must be employed rather than just targeting the strength of the right muscle or some theoretical movement ideal.
A recalibration process must also take into account the current state of the person to decrease the likelihood of simply reinforcing these protective responses. The term graded exposure fits nicely here I feel.
This maybe where relevant/meaningful/functional movement (scrub out the term you don’t like but hopefully you get the sentiment!) may come into its own.
A feeling of disability from not being able to do something surely must have a profound effect on someone’s perception of there own body. By asking to people to avoid these movements are we simply reinforcing the current situation?
Someone who finds moving into lumbar flexion problematic such as bending over to pick up their kids or do their shoe laces then bending/flexion will be relevant to them. This is a completely normal human movement that may be triggering the alarm system that has become oversensitive for some reason and can be maintained by negative connotations regarding bending.
To avoid the alarm you may want to reintroduce these movements slowly with a graded exposure. Perhaps at first by minimizing the contribution of the lumbar spine through movement integration and then exposing it to a number of different variations of flexion that the spine is anatomically capable of doing and does do on a daily basis.
This study found that flexing the trunk was actually associated with less lower back pain amongst blue collar workers *Click Here*
Hopefully we can do this while avoiding damaging language and reinforcing the beliefs that someone may potentially hold about the current state of their back.
Finally translating this in to an effective and practical self-management program to create longer term changes in perception should be the aim.
Robust
The aim of any progressive movement based program should be to take someone from a more sensitive state with regards to movement right up to a more robust state.
Robustness would be being able to tolerate changes in loading such as increased speed, weight, time (more), ranges of motion or positions. Someone’s back may not ‘go’ until they spend longer gardening or pick something up heavier than they are used to.
Subsidence of pain, which possibly will happen simply as a regression to the mean, does not mean that their physical capabilities are now increased and the same event won’t trigger the same response.
Often people get into a boom and bust cycle where certain activities or actions will cause them back pain. We could call these activities being outside of their ‘zone of homeostasis'. This could be large single events or an accumulation of repetitive events.
The ‘zone of homeostasis’ would include movements at ranges, weights, speeds, time frames and positions that caused no adverse responses.
The aim of rehab would be to bring these events outside of the 'zone' back inside the ‘zone’ by progressively loading relevant activities and variables to increase the size of the 'zone'.
Homeostasis of the organism has been a concept explored with regards to tissue loading (pathophysiological) by the surgeon Scott Dye and the endocrine system (stress system-allostatic loads) by Robert Sapolsky.
I think we also need to throw into the mix the response of CNS to loads outside of the perceived ‘zone of homeostasis’.
The perception of supraphysiological loading may cause a protective response based on the CNS’s interpretation of the current state of the organism and the context of the current task being performed.
Outside of a sporting environment perhaps there is less of a focus on increasing robustness where the gap between therapy and training becomes much smaller. The closer we get to the robust end of the loading scale it should just look like training for increased capacity and regular activity.
Please check out our 'Functional Therapeutic Movement: Assess & Rehab' course based on these concepts. *Click Here*












