The No1 way to move to get OUT of pain!
When you delve into looking at how people move you will soon encounter the murky concept of what is ‘correct’ or ‘good’ movement. This is generally coupled with strong beliefs in these concepts that are hard to shift regardless of the evidence.
Alberto Brandolini sums this up very nicely:
"The amount of energy necessary to refute bullshit is an order of magnitude bigger than to produce it”
While I do not agree that the idea of being able to define ‘good’ movement is total bullshit it has certainly proved to be an elusive endeavor and is very unclear so far. Based on the available evidence it would seem the best we can do in terms of rehabilitation and helping people move whilst in pain is to simply get them moving…. DIFFERENTLY.
A recent look at the FMS *HERE*, a system that attempts to provide criteria for ‘good’ movement and associated injury risk for ‘bad’ movement, found that the average score of the 74 athletes who got injured during the course of the study was 14.3 for the screens performed. The 93 uninjured athletes scored….wait for it….14.1 a whopping 0.2 difference.
The only movement pattern associated with injury was the in line lunge. The athletes who scored a 3 (the best score) were MORE likely to get injured than those that scored a 2! That is the more rigidly you can stick to what is perceived as a ‘good’ movement the more you are likely to get injured. In fact those scoring a 0 or 1 (the worst scores) showed no association with injury.
Moving IN pain
Any movement assessment of someone IN pain may only be a reflection of their response to being in pain NOT the reason why they have gotten into pain. This basic reasoning process is often not considered and provides a great rational for a movement change to off load an irritated tissue or to decrease maladaptive responses such as muscle guarding and stiffness later in a rehabilitation process. ANY movement can be used a screen or assessment for this purpose, the more relevant to the individual the better!
Movement assessment should focus on how you are moving RIGHT NOW regardless of whether that is right or wrong, especially when in pain, to give an indication of what to change and how to change it. Decreased ability to move differently and have other movement options has been associated with the transition from an acute injury to chronicity *HERE*. Decreased variation is strongly associated with chronicity when we use non-linear methods to assess movement *HERE*
Good movement, in my opinion, could be characterized by having movement options and bad movement could therefore be defined as having a lack of options.
One of my favourite sayings is:
“All exercise is movement but not all movement is an exercise”
Simply this means that any exercise can be adapted and altered to provide a less painful movement or movement can be used that does not look like ANY traditional exercise. Simply altering foot positions in a squat or a lunge will adjust femoral orientation in the acetabulum and provide a different stimulus to both the tissues of the hip and the CNS for a different response - hopefully less pain. All of these positions should be available within our movement repertoire for a sizeable capacity and available options to deal with varying situations and stimuli. We specifically adapt to the stimulus we are exposed to and therefore are more able to deal with the same stimulus in the future.
People are often uncomfortable with moving away from the exact invariant blueprint of how they have been taught or believe an exercise should be performed. Maybe it won’t target the same muscle or they believe it is less safe? If we look at less contrived movement such as in sport you will often move into these variations multiple times during a game. In fact you may not ever use the version you have practiced in the gym!
In a pain situation the aim may simply be to move with less pain rather than targeting a specific muscle to make it stronger. I would hope we are now moving away from a single muscle weakness as a cause of pain or biomechanical ‘dysfunction’
The more you move in the same way with pain the more you are likely to trigger the same response. The painful movement could look like ‘really good’ movement and ‘really bad’ movement could be pain free. We need to get MORE comfortable with being able to adapt exercises and movements to the person rather than shoehorning them into an ‘ideal’ version of an exercise.
Why does moving differently cause less pain?
Lets first think about what is going on in the tissue where it hurts although of course we cannot forget that the brain will also play a role in the modulation of any signal coming from the periphery. The science, which we will take a basic look at, is as important as evidence but less sexy it seems!
Secondly and perhaps more important when dealing with people in persistent pain states we must also consider associative learning and the coupling between non noxious proprioceptive stimulus and a pain response as well.
Nociceptors that encode high threshold noxious stimulus, or more plainly put danger signals, become MORE sensitive during bouts of prolonged firing and this decreases the amount of stimulus that is then required to activate them. They can be poly modal meaning they respond to a number of stimuli, heat, chemical and mechanical stimulus can all cause them to fire. All of these can be present during pain and inflammation.
So for a start simply moving in ways that have less impact on these afferent sensory neurons is a great place to start. Even finding joint positions that are less painful and can tolerate isometric loads can be a good way to stimulate an area to adapt without irritating it.
These first order afferent sensory neurons synapse in dorsal horn where the second order neurons are stimulated and throw the information upstairs to the brain. Prolonged stimulation via an impulse barrage from the periphery can cause increased excitation of the spinal cord neurons that may start to increase their receptive field; this activity can also start to excite neighboring synapses as well. This is often referred to as ‘wind up’.
Even in an acute pain situation these changes in the central processing of pain can alter or may have been altered by previous painful experiences. We often associate central mechanisms with more chronic pain states but central mechanisms will always be involved in any pain so the possibility of more central involvement is always present. If someone has had a history of pain refractory nociceptors that have previously been quiet or silent may subsequently become more active and add to this process. We may also have receptors that previously had a normal sensitivity state that now are more sensitive to future stimulus.
Once these receptors are turned on they may stay switched on for a while or never totally switch off. C fibre information travels slowly due to the lack of axon myelination so signals from the peripheral terminal endings may take some time to get to the CNS and then also some time for any inflammatory responses produced by the cell body or dorsal horn to get back down there. So as more C fibres wake up and start signaling then this probably goes some way to explaining why pain often hurts the next day and can carry on for a bit afterwards. This also helps us to understand why that fine line can sometimes be crossed in rehab when we do a bit too much in a session and it is not until the next day we become aware that the threshold has been crossed and triggered the alarm.
Part of making the alarm system of pain better, often a maladaptive response, is making the sensors more sensitive to better detect a stimulus. Once we understand this it makes complete sense why pain can easily be triggered in some people especially if they have a history of pain or injury.
Essentially some peoples CNS’s get very good at being in pain! So pain is very easy to trigger and because it is easy to trigger people become both aware and wary of this. We see this with hyper vigilance and fear avoidance. Being able to find pain free movements with these people becomes of huge value far outweighing if it is the ‘right’ exercise performed in the ‘right’ way. If we can also make movement relevant to the person then the psychological value is going to be significant. Fear avoidance is in part is maintained by avoiding perceived pain situations and therefore not getting pain, the relevance of movement and the dosage of how we interact is paramount. Not addressing relevant movement may sustain the problem.
The whole idea of helping people move differently and with less pain is to maintain moving while not triggering or adding to their current pain state. Getting comfortable with an idea of the biochemistry being a factor as much as the biomechanics is a step in the right direction. We can in fact use different mechanics to drive different chemical reactions.
Movement is good!
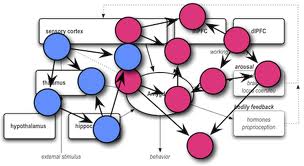
Movement also promotes basic fluid dynamics that can take away the nasty stuff and bring in good stuff so not moving is generally not the answer. Movement is also analgesic *HERE* An increase in corticomotor output promoting descending inhibition and an increase in endogenous opioid production have both been discussed as potential mechanisms. The more inhibitory chemicals we have floating around the spinal cord the less sensitive it is likely to be, this includes chemicals such as GABA and endogenous opioids. This top down inhibition can influence what’s happening physiologically within the tissues and even simply having positive associations with movement may have an inhibitory effect on pain.
Stiff tight muscles and complete off loading may only add to the problem. We have acid sensing Ion channels (ASICs) and TRVP1 channels in our receptors that both sense decreased PH caused by ischemic tissue states arising from prolonged positions or postures and this may add to increased local sensitivity. Using our bodies as normally as possibly will also reduce deconditioning and maintain movement ranges and tolerances.
Sensitisation
It is not just the CNS that can become sensitized. The peripheral neurons can also become more sensitive by manufacturing more Ion channels up in the cell body and then popping them down to the terminal ending in the tissue. This increase in Ion channels makes it easier for more positively charged stuff outside the cell to get into the cell to depolarize it and then send a signal up towards the CNS. These could be mechanically sensitive to stretch or ligand chemical receptors. Ligand receptors have chemical receptors built into the ion channels that open in the presence of specific chemicals such as are present in inflammation.
When the afferent sensory C fibres fire their orthodromic (towards CNS) message off to the dorsal horn they can also causes an antidromic (towards the periphery) impulse back towards the terminal ending and associated tissues, this called neurogenic inflammation. This stimulates the release of neuropeptides including substance P and CGRP that further irritate the local area causing things such as mast cells to degranulate releasing histamine and serotonin creating a pro inflammatory and nociceptor sensitizing soup. In between the orthodromic firing somehow the cell can also manage to send a barrage the other way as well. What a busy bunch of neurons! We can have central to peripheral activity from the dorsal horn as well through the dorsal root reflex.
This process will be certainly be influenced by people’s individual nervous systems, physiological responses and previous pain experiences that may have altered their physiological responses.
So essentially a mechanical force could create an noxious afferent signal towards the CNS also triggering a local inflammatory response further sensitizing the chemically sensitive receptors or receptors that are affected by both chemical and mechanical stimulus thus making them even more sensitive to movement. A loop hopefully broken by finding some pain free movement.
This is all getting quite complicated by hopefully should give us an idea that getting people moving and simply moving differently to the way they are right now rather than any ‘right’ way will probably help out with all the pain biochemistry going on in their tissues or the changes that can occur further up at the dorsal horn by stimulating different tissues and receptors. We can desensitise by not further sensitising through repetitive receptor stimulation as well as also stimulating the descending good stuff!
Non nociceptive mechanisms
Hypotheses are now emerging that look at the association of non-nociceptive information and pain. I have previously discussed the concept of pain memories in more detail *HERE*
With this line of thinking we have the association of two encoded stimuli, one being pain and the other specific proprioceptive information generated via a specific movement. Over time they may have become coupled in a neural pattern and the proprioceptive information can become a stimulus for a conditioned pain response. No actual noxious stimulus is now needed to elicit a pain response. This makes a lot of sense with reagrds to conditioned fear and apprehension behaviours present in lots of persistent pain sufferers that have experienced pain that far outlasts weighs tissue healing times. These ideas are certainly not new in the world of emotional research where they look at conditions such as fear conditioning.
Moseley and Vlaeyen *HERE* have put forward the ‘imprecision hypothesis’ that discusses how pain can be generated by a wide array of movements and activities. These neural associations between movement and pain can become pretty generalised rather than specific and precise. This means that a stimulus in a similar kind of ball park or of a similar type might start to trigger the conditioned pain response. This can be problematic as multiple loosely associated stimuli can now cause pain. This increased protective buffer probably serves a good adaptive purpose at some point in a more acute stage but less so later down the line when it transitions to being maladaptive.
So here we would hope different movement causes a different proprioceptive input to the CNS that is not coupled with pain and therefore generates a different output response namely no pain!
Although modifying how someone feels is great we cannot forget that pain alters movement as well as tissue sensitivity even after the pain subsides. Both may add to reoccurrence and possibly why the best predictor of future injury is previous injury. Protective movement behaviours should also be dealt with during any rehab process. Not rights and wrongs but instead a variety of movement options and skills should be introduced so the system can adapt by being able to have more variable resources.
Thanks to Butler, Gifford and Shacklock for providing the good science!













Leave a Reply
Want to join the discussion?Feel free to contribute!