The perspective that the body is an interconnected unit that displays regional interdependence is a valuable one. That different parts interact in different ways during different activities and influence ROM (range of movement) in other areas of the movement chain should seem a fairly easy link to make when looking at the whole body during different context dependent movements. We often eschew the value of the integrated system in favour of the isolated joint/muscle model.
Read more
Posts
So I have seen various variations on Gary Gray’s view that muscles are reactors. I think this is spot on. Muscles ARE reactors.
I think what Gary meant by this was that generally we see muscles as concentric force producers. Actually during movement we tend to need to decelerate motion by eccentric contraction first. Think walking first we flex to attenuate gravity, ground reaction forces, mass and momentum before creating force to move. So we are reacting to forces acting on the body before we create concentric force.
Read more
One of the key things to understanding how to view the body functionally specific is the biomechanics behind how we move.
A (simplified) understanding of biomechanics allows us to break down different functions to create authentic movement based techniques that create the right joint reactions for when we are training or treating our clients. After teaching a mentorship group last weekend some of Cor-Kinetic’s principles of biomechanics I thought I would write this blog post to help explain our process that has also been influenced by the teachings of the Gray institute.
Now the word biomechanics sounds a bit scary. If you have ever opened up a biomechanics book or journal then you will probably have had a similar reaction to me, which is one of amazement at the equations and symbols on offer!
(Apparently the biomechanics behind swimming!)
Instead in the process we use at Cor-Kinetic we are looking more at the movement of bones both in real space and in relation to each other. This relative movement of the bones creates specific joint reactions that in turn will have an affect on the attached muscles for an authentic reaction in the neuromuscularskeletal system as a whole.
The real key is in understanding that the real bone motion and relative joint motion can be different. So in essence we could have two bones both externally rotating in real space but the relative motion between the bones at the joint could be internal rotation. This hinges on the difference in speed between the two bones. Lets outline some of the key points below.
Proximal and Distal.
It is key to know which is the proximal and which is the distal bone at a joint.
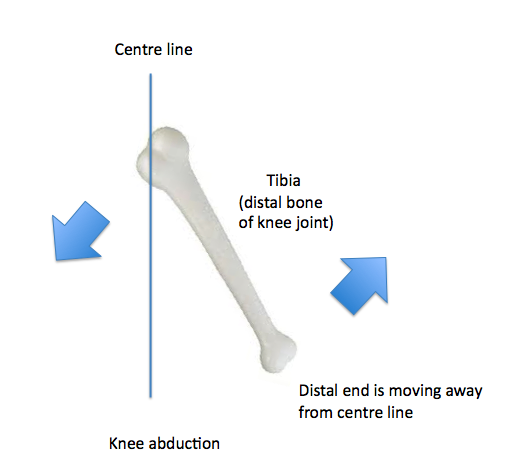
In the appendicular skeleton (extremities) the motion the DISTAL end of the DISTAL bone is going through RELATIVE to the PROXIMAL end determines joint motion. This means if the proximal end is moving towards the centre line in the frontal plane for example then the distal end will be moving away or abducting!
The distal point of the Axial skeleton is also known as the superior point. So now we look at the superior point to define joint motions at the axial skeleton.
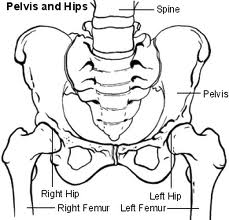
The proximal bone is the one that is closest to the centre of the body. Therefore the pelvis would be the most proximal bone of the body. The other bones are distal to it. That makes understanding the proximal and distal bones of the hip joint easy as the pelvis is always proximal. At the knee the femur would be the proximal bone to the distal tibia.
The motion of the pelvis is also determined from a different point. Rather than the distal end (because both are!) we look at the relative movement between the ASIS and PSIS. Anterior rotation would be the counter-clockwise rotation of the ASIS so the PSIS would be superior to the ASIS.
The same counter-clockwise rotation as we see from the tibia would be described as posterior rotation because the distal end has rotated towards the posterior. This can sometimes be confusing because both the tibia and pelvis bones are going through the same rotation but one is described as anterior and the other posterior!
Relative speed.
The relative speed of the two joints is also critical to determining the relative joint motion.
It is important to now know which bone is moving faster as this will help to determine the relative joint motion. The general rule is that the closer the bone to the driver of motion the faster it will be going. This is because of the dissipation of force. As an example, a foot driven motion will generally mean the distal bone of the lower limb will be moving faster. So at the knee the tibia will be driving faster than the femur. If we were to hit a tennis shot however the proximal femur would be closer to the driver of the hand meaning it will be moving faster. At the elbow however the distal radius would be closer to the hand meaning it would be driving faster than the more proximal humorous. So we need to know the driver and which of the bones that comprise the joint we are looking at is closer to the driver.
There are 3 real ways a joint can move in function (and two more less functional to make 5). This would be proximal and distal moving in the same direction, proximal moving faster. Proximal and distal moving in the same direction, distal moving faster and then proximal and distal moving in opposite directions. This would be either towards or away from each other as if we view a clock face movement towards each other would mean one was moving clockwise and the other counter clockwise this would be the same when moving away from each other also!
This is all very easy when the distal bone is moving faster as the real bone motion and relative joint motion will be the same. The confusion comes in when the proximal bone is driving faster than the distal in the same direction. In this case the relative joint motion will be the opposite to that of the proximal bone. An example in the transverse plane would be at the hip in the back leg of gait. Both the real bone motion of pelvis and femur is rotating in the same direction, externally. However because the proximal is rotating faster the relative joint motion is internal rotation. The easiest way I find is to put my fists on top of each other. I then rotate the proximal bone in the direction it is rotating, in this case external. I then rotate the bottom hand in the opposite (what determines the joint motion) and this is internal! The transverse plane can be easier to understand sometimes because the whole bone will be rotating in the same direction rather than the proximal end one way and the distal end the other!
One movement that can sometimes be confusing is abduction of the knee. This is because the largest motion is from the proximal end going towards the mid-line, rotating around the axis that runs posterior to anterior. But if we follow the rule of naming the joint motion from what the distal end of the distal bone is doing relative to the proximal end, then it is moving away from the centre line of the body or abducting! Easy when you know the rules!!
Check out www.cor-kinetic.com for more information on our courses.
As always this is an example of our thought process rather than a defined way that things have to be done in an academic sense! We hope it helps!
I have read a lot of stuff on movement screens recently and specific "functional tests" such as overhead squats and single leg squats. People both extolling their virtues and others maybe less sure about their validity.
I thought I might chime in with my thoughts on these "screens". Firstly part of the problem is we are trying to shoe horn function into a handful of assessments. Given the incalculable number of functions this is a pretty tall order. Another problem is that we are trying to 'define' Peoples function. This has always been the problem with 'functional' training, trainers tend to define the clients function rather than the other way round. A more successful approach, although less easy, is to have a thought process that allows us to understand the biomechanics behind someones function and be able to design a test to tell us how well someone interacts with their functional activity. At Cor-kinetic this forms a cornerstone or principle of how we approach the body and teach people to approach the body.
So are you testing the test? Or are you testing someones functional needs? That is a question you have to ask yourself! If the test has nothing to do with the needs of the client or player then what validity does the answer have? We are simply testing a test.
All movement is a specific skill. Many sporting movements are very specific skills honed over a number of years. Is a poor test on a movement we have not practiced just poor skill at the movement as we have spent no time refining it? Are the improvements in the movement skill based? If so then would it not be better to spend the time practicing a skill that we really need for our sport? These are all questions we need to ask.
As movement patterns live in the brain and we have between 100-120 billion neurons each with around 10,000 connections each I am pretty sure we have the neural real estate to hold more than a handful of movements that define how we function.
Does a tennis look like rugby? If not then we need to find a way to screen them specifically.
The single leg squat test does go a little way to incorporating a functional thought process. The fact that a person during gait spends between 50-85% on a single leg depending who you listen too has a sprinkling of specificity. I think more towards the first figure for walking and more towards the second figure for running! However the amount we squat during walking gait would be minimal.
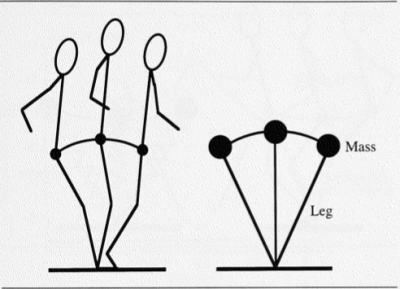
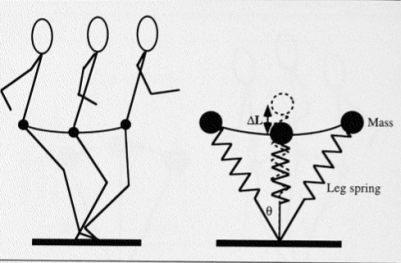
This is the inverse pendulum model of human walking gait, this means we are able to be efficient and use gravity to transfer our COM (centre of mass). This is in opposition to the spring mass model of running. The aim of walking gait is to not overly squat and lower our COM. (Farley 1998)
So a single leg squat maybe more 'functional' for running but not walking gait. Although the depth of the squat may still not be large. We can see the variation in function here and a single test to define our 'functionality' may be of limited value. A much more valid process may be to understand the variation in function of the client stood before me.
The major factor in both functions (walking and running) is being able to effectively move our COM. The ability to translate as well as rotate is a massive component of human movement. Nearly all 'functional' tests seem to assess our ability to move in the vertical component of the sagittal plane rather than the horizontal which is at least as important if we ever want to get any where. The art of transferring and controlling our COM dynamically should be a principle part of any 'functional' testing screen or protocol.
This is something that the S/L squat does not tell us but is one of the most important 'functional' tests we can have. Also would a more effective adaptation to a S/L test to find out how our pelvis is able to rotate over our femur creating relative IR at the hip whilst in a S/L stance?? This would be more 'functional' for both walking and running. The stability we crave in a S/L stance maybe generated through eccentric tension of the numerous external rotators and adductors (many of which are lengthen in IR)! Without the pelvic rotation this stability could be compromised, so testing stability without pelvic rotation on a S/L for gait maybe a bit like a driving test with 3 wheels!!! Function is specific and if we want to be 'functional' we must learn to be more specific also.
An overhead squat test is another 'functional' test and very rarely in functional activity do we do things bilaterally or over head for that matter!
If we go back to the pretty universal function of gait, we can see that the two arms are doing different things. One is flexing, one extending. One externally rotating, one internally. This means that the scapulae will also be doing different things. elevating and depressing, retracting and protracting. In fact any function which involves rotation (pretty much all of them!) this will be occurring at the glenohumeral and scapulothoracic joints. Can a test that fails to take any of this into account be reliable for predicting any movement pattern dysfunction in the body away from a single plane overhead squat?? In everyday function we rarely squat from a contrived position defined by someone else. Squat down to do the gardening or get something from the fridge I guarantee it will not be in the pelvic neutral, toe out and linear fashion we do in the gym. To assess and train like this and define it as 'functional' may not be accurate in both thought process and application. The variation in foot position, and therefore hip position, in all three planes in functional squatting is huge. Dysfunction or pain could be occur away from this one contrived position and a thought process that allows us to test a wider variety of positions in a movement may give us more information.
Lastly muscular range in one plane of motion may be naturally mitigated when three-dimensional tensile or compressive force is acting on the fibres. Simply a structure may not be able gain as much length in one plane when also being pulled in another direction or plane. So a test that only tests a single plane at a time may also give information not consistent with three-dimensional functional muscle movement. This is similar to single plane force production (isolated) not being applicable in a three dimension environment where force has to balance across three planes.
As always this is my opinion on a complicated subject that has no definitive answer, only more questions!!!
I have read a few blogs recently on fascia. All of them giving a different perspective on what is a very prevalent topic at the moment.
One was based around the significance of fascial contraction and the biomechanical influence it could exert on the body. This made me think of the a pair of articles and an audio presentation I wrote for PTontheNet. In these articles I posed the question "how would fascia contract".
As far as I am aware fascia seems to mainly afferent, sending information to the CNS, rather than being able to efferently regulate tension through the feedback loop of muscle spindles and motor units. So if fascia does actively contract then why and is an active biomechanical influence helpful??
Chemical contraction has been noted in vitro (out of the body) in rat fascia (schliep 2006). These changes in response to chemical factors were in this case due to calcium chloride, calcium being involved in both skeletal and smooth muscle contraction although in different ways.
I think the link between the biochemical and biomechanical is an important one. Stress creates significant biochemical changes in the body. Hormones associated with stress such as cortisol are also involved in energy regulation. The body in response to long term stressors and increased energy expenditure may choose to decrease movement to conserve energy. This could be looked at as another way of interpreting the law of energy conservation on a metabolic level!!
One way of decreasing movement could be to increase the stiffness of the body. Fascia in its various forms being ubiquitous in the body could certainly play a role in this longer term stiffness regulation that would require less instantaneous neurological control than involved in active muscle contraction.
Now this maybe good for the body on one level (energy), maybe not so good on another (movement). So the biomechanical impact of stiffness regulation for fascia may be detrimental for our movement, especially if it becomes a learned response of the body and becomes the 'default' tension even when under less stress as I believe can happen.
Some may argue that increased compression through contraction of fascia at the lumbar spine is helpful. However this may not be the case if the movement at our hips is also reduced. The ball and socket joint of the hip is designed to have a large movement potential especially in the transverse plane. If this motion is reduced, through fascial stiffness, more motion may have to come from the lumbar area to achieve function related movement. Lumbar rotation is limited (by facet orientation) to 5 degrees collectively in all the 5 vertebrae!!
This could be a recipe for increased articular surface compression if the superior segment rotation (driven by top down movement) is not in close sequence with inferior segment rotation. If both rotate similar amounts then less compression. If one is blocked then this will increase compressive force between the two segments. If we put our hands one in front of the other and rotate them together we feel less compression. Try moving one and keeping the other still, this will increase compression. If the pelvis is not able to rotate on the femur then the inferior lumbar segment closest to the hip will be blocked. This will lead to increased compressive forces and possibly also to pain!
It does however give an insight into why some people have chronic movement dysfunctions that cannot be treated by biomechanical intervention alone without looking at biochemical, nutritional or emotional factors.
I also think we overlook the passive role that fascial stiffness plays in the body. Is passive resistance to movement as important as active contraction?? I personally think so. Our passive stiffness controls the range, speed and energy consumption of our movement. This seems to be overlooked in a similar way to eccentric muscle contraction controlling our movement by decelerating our momentum and controlling forces.
The differing types of collagen contained in different fascia may give slightly different interactions with energy. Some stiffer varieties maybe able to store and return energy whilst others may exert their stiff properties before plastically deforming and having their shape reset by muscle force.
This model would be quicker and more energy efficient than active contraction, neurological or chemical. The force of the movement (hopefully) dictating the correct response of the tissue.
As always this is merely my simple opinion on a complex clinical subject. I have also tried to give a perspective using a functional movement context.
Ben!!
Its been a while since I last wrote so I thought I better had! Today's blog is about dynamic stretching.
To stretch or not to stretch, dynamic or static, these are all questions posed in the fitness industry. Another question is does stretching reduce injury?? This is not a question that I want to get into but instead look at stretching as improving our exercise experience and performance. For me, if we want to increase movement we do this by, increasing movement.
First of all I think we see stretching as a mechanical experience that increase tissue length. To some degree this is true. However I also see dynamic stretching as a neurological experience that increases information flow around the body. So many of the bodies receptors that live in the skin, fascia, joint capsules and muscles respond to change. This would be change in angle, length, tension, pressure and vibration to name a few. Dynamic movement creates constant change, a static change of position only creates one change!
By increasing the movement sphere and therefore information sphere we increase the potential for more movement. As movement increases, so does the ability to increase the range or sphere. A good friend of mine coined the phrase "movement begets movement" I think this is pretty good way of summing this up! So by remaining static we will not increase this sphere or give the body the potential to increase the sphere.
If we look at the information mechanisms in the body and were to look solely at muscles for this information the muscle spindles would be a great place to start. The spindles have two types of Efferent (info towards the brain). One is based on tissue length and one is based on the rate of change of this length. These intrafusal fibres are vital for the feedback loop, through the gamma and alpha motor neurons, that then regulates the stiffness (resistance to lengthening) of the extrafusal muscle fibres and hence successful movement.
By statically lengthening the muscles we are only giving half of the picture. Movement requires both length and rate of change of length information to be successful. Imagine having the GPS system of your car only relay half the information, and the bit omitted was the speed you were traveling at. I think you would be missing a lot of turns!!!
We also tend to only stretch along the fibre direction or longitudinal axis of the muscle. If we look at the mechanical nature of the spindles then this would lengthen and put the spindles under tension but also imagine that when under longitudinal tension adding in perpendicular and rotational tension. This would affect the information flow also. This demonstrates from a muscular perspective why three dimensionality and movement are pretty vital to the stretching or movement enhancing process. Especially as functional movement uses all three planes!
Also we must see stretching as an integrated procedure. In an integrated system such as the body the range of one joint maybe inhibited by the range available to another. If we stretch the joints separate of their function specific chain we may get a different ranges to if they are integrated. In fact a smaller individual range but a larger integrated movement may be the best desired outcome for some joints to avoid tissue stress.
Many factors may also affect the flexibility of the body. These could be stress, diet, disease and eyesight to name a few. If we can understand the feed forward mechanism of the gamma motor neuron upregulating the stiffness of the spindles and therefore the alpha motor neuron changing the stiffness of muscle fibres, it is easier to see why the above stressors of the system can have such a huge impact on flexibility and therefore the biomechanics of the body!!
I have never understood how remaining still will help us move!!!
This blog comes courtesy of a conversation I had with my good friend Mike. Its all about optimum range of a muscle. It kind of followed on from this piece of info…
The eccentrically-loaded muscle will start its contraction weak and then get stronger; the concentrically-loaded muscle will initiate strong, but get weaker as the contraction continues.
I had never given this much thought before but this makes a lot of sense when we think of length tension relationships. A muscle will struggle to produce force when both too long and too short. Being weak in both positions. Cross bridge attachment has an optimal range. This will be true of both force production and conservation of energy. Too much cross bridge detachment will also cause a more thermodynamically expensive scenario as we split ATP and dissipate energy as heat.
Elastic energy will also I believe have an optimal range. Studies have shown that spring stiffness (ability to return energy) comes from optimal joint angles or ranges. Going beyond this range means that we dampen or absorb energy, again dissipating as heat through visceoelasticity of tissue. Different tissues have varying levels of stiffness and compliance, different ranges will bring into play these different characteristics as will our neurological intention (land or jump again) to move control stiffness through efferent spindle stiffness regulation.
If we look at the way we jump when we want to jump again, we can see that we use a shorter joint range than when we land for the final time. When we finish we have a large bend of the knee to absorb ground reaction forces rather than reuse them. This has implications for our understanding of height, range and repetition programming for our training me thinks!!
Ecconcentric (both eccentric and concentric muscle contractions occurring in different planes) muscle action may also play a role in optimal cross bridge attachment. If a muscle was to lengthen in all three planes this may cause a scenario where we are going beyond the optimal range for the muscle in terms of force production and elastic energy recoil. By mitigating elongation of the tissue in a plane of motion through concentric shortening we may also keep an optimal range. It maybe this would happen in a more sub maximal scenario where energy return and energy conservation are more important than maximal force production. I feel that gait is a great example of this. Although maximal force production may also be mitigated by creating too much loading through joint range that is hard to transform.
This then got me thinking about how we train. Many times we are looking for maximal ranges in our training. Maybe we should be looking more at optimal ranges. This may have more implications for sports where we can control the range through skill however. Running is a great example. Controlling stride length will keep us within optimal joint ranges. We must also remember that optimal will be governed by the individual. This will be affected by tissue ability, limb length, speed ability and event. I expect it will be that different events within running e.g. 400 metres will need different joint ranges from a marathon as we balance need for all out power, power-endurance and endurance. Going beyond optimal means our ability to start the next phase of movement, either eccentric to concentric or vice versa, will be compromised. I think that deceleration and acceleration are part of running (unlike the pose method ideology!) However we can mitigate excessive amounts of both having to occur, increasing energy conservation.
If we look at a game of tennis it is much easier to hit a powerful shot when we can manoeuvre our bodies into position. When we are out of position our range of movement may have to be extended to reach the ball. The transformation from eccentric to concentric is sub optimal and affects the power of the shot. The tennis player many times at end range will hit a defensive shot back, aiming to get it in the court rather than a winner! Increases in amortisation from eccentric to concentric reduces cross bridge attachment also decreasing energy return. The closer we get to and stay at end range stretching for the ball the longer we have the amortisation phase reducing the energy gained in the loading motion.
This is a very theoretical piece and mainly my own thoughts (so blame me!!) but it may give us food for thought when we programme ranges/heights for our clients to move through when training.
More may not be better in all circumstances!!!
Latest Articles
 If 9 out of 10 interventions are a load of rubbish, what the hell do I DO?August 4, 2022 - 3:29 pm
If 9 out of 10 interventions are a load of rubbish, what the hell do I DO?August 4, 2022 - 3:29 pm Why the advice to “rest” & “remain active” can both be a bit rubbish!December 21, 2021 - 2:38 pm
Why the advice to “rest” & “remain active” can both be a bit rubbish!December 21, 2021 - 2:38 pm Why I HATE discussions about treatment…….June 22, 2021 - 6:58 am
Why I HATE discussions about treatment…….June 22, 2021 - 6:58 am Evidence based practice – Do you love or loathe it?March 29, 2021 - 3:09 pm
Evidence based practice – Do you love or loathe it?March 29, 2021 - 3:09 pm- The myth of exercise prescriptions – It’s probably more trial and error than we care to admitOctober 15, 2020 - 11:43 am
 Education in rehab – WTF does it mean…..?October 1, 2020 - 12:15 pm
Education in rehab – WTF does it mean…..?October 1, 2020 - 12:15 pm
SIGN UP FOR UPDATES