I know, I know, it’s a sensational title but what did you expect, it’s social media 😀
But it’s pretty depressing when you read papers like this one that recently was published regarding how effective many treatments are in healthcare. 9 out of 10 are NOT supported by high quality evidence *HERE*
There is a ton of research that doesn’t show amazing results and many interventions don’t reach a minimal clinical important difference (MCID) threshold of 1 to 2 points on a 11-point scale (depending on the comparator). This for me is NOT surprising as there are so many things outside of patients and therapists’ control such as lifestyle, genetics, social determinants of health, comorbidity, and the natural history of a condition not to mention the fact that pain is just an elusive muthafunker.
But before you get too down in the dumps, it is important to remember that people also do get better *HERE*, it may not just be the specific interventions we use that do that, even though some people can mistake this for their own brand of magic *HERE*.
So, if we are being evidence based then what do we do now? Spiralling into a sea of intervention ineffectiveness depression is of course one option but it’s not recommended for any length of time.
As Voltaire eloquently told us a few years back….
“The art of medicine consists of amusing the patient while nature cures the disease.”

If I were to give that phrase a 21st century update, it’s not so much about amusement but more about understanding and sense making, reducing the worry and anxiety that can often amplify the problem *HERE*
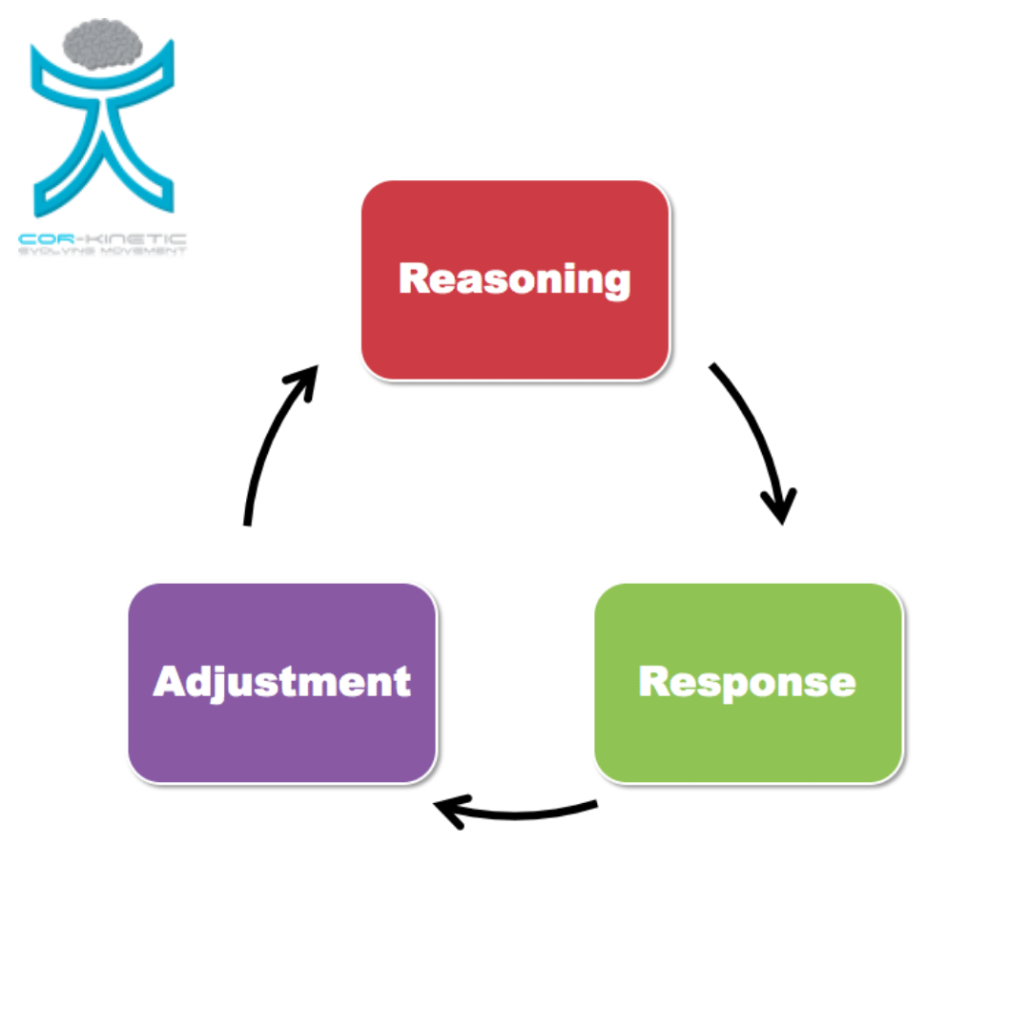
Let me state this clearly, the point here is NOT to offer this up as an alternative nirvana of treatment that outperforms what we have in terms of current research, I can hear it now “show me the data” (think Jerry Maguire). It’s actually working within the research base we have currently and accepting the lack of treatments that have a large effect. Being a clinician (and a person) is mostly about acceptance in my experience 😀
This for me is a very undervalued part of working with people with painful problems. How do we measure or quantify it? Not really sure (I will leave that to smarter folk than me). Do we need to? Depends on your point of view. Should we do it even if it does not improve outcomes? I think so! Part of the point of the BPS model was to move away from everything being quantified or put into little boxes.
This recent paper points clearly to people with back pain wanting to understand more about their issue *HERE*
How can we do this?
Firstly clinicians understanding the problem really helps! That way we can un pick all the silly bullshit that exists around many MSK issues. So the “muscle is not activating” or “this muscle is tight” or “bones out of alignment”, I don’t need to tell you this as you probably hear it every day. Back pain is literally a pandemic of bollocks and bullshit. You cannot do this if you don’t understand the problem to begin with and there is huge value in not making the problem WORSE.
Giving accurate and realistic information to help make sense of the issue, for me, is a big deal and major part of helping people. That last word is important, PEOPLE not just pain. Remember we discussed how elusive pain is at the beginning (and that’s EVIDENCE BASED).
It’s not just knowing about the problem and then vomiting ‘education’ all over people, it’s also about understanding what is worrying them and what they would like to know more about. How can you reassure for example if you don’t know what someone is worried about? You can certainly dump information on people and hope it has an effect or you could ask!
This is all really improved if we can connect (as much as possible) and see the value creating a space for open and honest dialogue. This is really the special sauce in working with people, especially if the interventions are not quite there yet.
I have come to see the treatments applied as only part of the value that I and others have to offer. Especially given the data around effectiveness. The process of interaction, communication & sense making should be seen as just as important even if if doesn’t have a huge effect on outcome measures such as pain & disability (in my opinion of course).