Here is a short video I did on the Rethinking physiotherapy Facebook page on Applying pain science education. ENJOY!!!!
Pain education is a valuable tool for some, but certainly not all, patients. It can help to provide a narrative or explanation for problems that may remain unexplained by ‘traditional’ medicine or therapy.
This paper HERE regarding chronic lower back pain explores what people are looking for from a visit to a therapist.
“more than 90% of patients expected a physical examination, tests or investigations, a diagnosis, reassurance and advice, and clear explanations of causation, symptom management”
How tough is this in many instances with no clear diagnosis or causation available?
Up to 90% of back pain is described as ‘non specific’ for this very reason. We know that uncertainty is a big deal for many patients. Mishel first proposed this in the “theory of uncertainty of illness” HERE.
Carroll's paper HERE “How Well Do You Expect to Recover, and What Does Recovery Mean, Anyway? Qualitative Study of Expectations After a Musculoskeletal Injury” also discusses the process of diagnosis, uncertainty and the subsequent effect on expectations of recovery.
But although data suggests pain education can help it can also be very tough to deliver.
This quote from Louis Gifford sums it up nicely.
"The patient that learned from their pain explaining therapist that their pain didn't really mean anything, who suddenly got out of the chair, went home and went riding their bike for the first time in 5 years...just doesn't really exist!”
So how can we improve the delivery of pain education?
A question I often ponder is have we replaced anatomy with neurobiology? Do we now bombard people with complex processes involving brains, nerves and receptors rather than complex biomechanical stories? How much neurobiology or neuroscience is actually required?
In some cases certainly it will be useful, but in many cases maybe it could actually hinder. This does not mean that some of the key concepts such as plasticity, sensitization and the brains role in pain are not important but maybe the minutia of information that can be focused on is unnecessary.
Perhaps we can apply some of the information in this paper HERE. Simplifying MRI reports appears to have a positive effect on how they are received. This may also apply to the delivery of pain education. What does nociception or Ion channel mean to a patient? It could end up very similar to VOMIT (Victims of Medical Imaging Technology) HERE if poorly delivered.
Should the focus now be on the delivery and context of information rather than the information itself?
Contributions
I thought it might be nice to get some other opinions on some of the key elements that go into making successful pain education and reached out to colleagues from around the world, using social media, to pitch in.
Some of the key components I already advocate, but I must admit some others I had not considered and provide valuable food for thought for myself and perhaps also the wider therapeutic community.
I was pleasantly surprised by the elements discussed, almost none related to the actual information itself but instead on the delivery and thought process involved.
Here they are!

Listening
The most consistent point made by the contributors as a whole was listening.
Listening is a key clinical tool. Although pain education is often thought of as the delivery of information, it should start with listening. I think this is advocated on many fronts but as we know patients can often be interrupted pretty quickly HERE and this is always worth keeping in mind.
The desire to be listened to also appears to be valued from a patient perspective and helps to build therapeutic alliance HERE. This is probably vital for those receiving and processing the information. delivered.
This is a good paper on ‘listening as therapy’ HERE
Validation
A couple of patients also contributed to the discussion and they felt that someone listening to and validating their experiences was a big part of their recovery. This also ties into the paper above regarding a patient’s perspective. If symptoms cannot be ‘medically’ explained or solved by traditional interventions, then patients may feel that they are being seen to ‘make it up’ or exaggerate their painful experience. All pain is real and although it can often be hard to describe it is also exactly the way that someone says it is. It cannot be anything else!
Individualisation
Another of the key points consistently put forward was about individualizing the delivery and placing into a relevant context. Now I personally have a bias for placing pain education in context with someone’s current situation. By weaving it into their story and using their painful examples to tie in some of the key concepts I think we are more likely to get some elements of comprehension.
This fits well with the key component of listening. Without listening we cannot place the information in the context of the patients narrative.
The question is, is this more effective than information generically delivered? I just don’t know. I think this would be an interesting comparison to study.
Asking!
One thing I must admit to NOT asking was simply “do you want to know more about pain?” This was brought up by a number of people. This may avoid the very real problem of ramming pain science where it is not wanted. Pain science should be judiciously applied where it is needed AND wanted rather than a therapist dropping knowledge bombs expecting an instant epiphany.
It is not a passive exchange
Remember there are two equal people involved in this. It is not simply a teacher pupil relationship. Patients lived experiences are also important. The therapist can also learn from the patient, especially when it comes to the patient experiences. Perhaps it should be seen as a journey by two people to find mutual meaning in a negative situation rather than simply an educational experience.
Pain science is a way of thinking not an intervention
One of the criticisms that I have seen recently of the application of pain education is that it is seen as a standalone intervention. So rather than bombarding people with statements or analogies that have been previously heard for explaining pain, the concepts and ideas should affect the way we reason, interact, explain and apply the treatment provided.
Experiences are as powerful as talking
It’s not just about talking; doing is also a powerful educator. Perhaps sometimes talking is needed before and after the doing, but without the actual doing we cannot ‘prove’ the point. Beliefs about the body are a good example of this. Without SEEING or FEELING a different, positive outcome to that expected, potentially a number of times, a belief may remain in place.
Again listening is key. What are the key experiences that need to be reconceptualised in a physical sense as well as a cognitive sense.
Find out HOW your education has been interpreted
As with any part of the therapy process, pain education has the potential to have a NEGATIVE outcome as well as a positive one. We may well baffle people with talk of brains and outputs etc and HOW they interpret this information is the arbiter of success, however well meaning or comprehensive the input by the therapist.
This may boil down to wording, health literacy and therapeutic alliance. The list of potential influencers is endless, but essentially the ability to mitigate any negative effects could be dependent on simply asking!
We may be able to influence this interpretation by being clear and concise, using bite sized chunks of information, avoiding confrontation regarding beliefs and also avoiding negative or long winded medical or anatomical jargon and terms.
Reflective questioning
Don't just providing statements, also use reflective questioning. This may help to facilitate understanding and apply this new information to their own personal experiences and think critically about some of the beliefs they may hold.
Lets say someone has a negative belief regarding about their back because of a slipped disk a number of years ago. We could suggest that structure and symptoms don’t always display a consistent relationship. We could follow this up by asking if their symptoms come and go (as long term back pain generally does) and would this be a sole cause if the ‘slipped’ disc remained a constant.
Of course this is just some opinion/s but collectively they could be valuable!
Key points
- People are looking for answers
- Uncertainty makes things worse
- Pain education may provide some explanation
- It is tough and often fails
Some things may make it more effective
- Listening
- Validation
- Individualisation
- Asking If it is wanted/needed
- It is not a passive exchange
- Pain science is a way of thinking not an intervention
- Experience is as powerful as talking.
- Find out HOW your education has been interpreted
- Reflective questioning
Here is another webinar! This time for the Pain Masterminds Network.
The subject is 'Exercise and clinical reasoning - More than sets and reps'
I am taking a look at moving beyond the tissue and capacity model of therapeutic exercise.
Below is the PDF of the presentation!
If I had a £ for everybody that mentioned posture on social media or when they had a pain problem…… well lets just say I would be a pretty rich guy.
POSTURE has literally become engrained in peoples thoughts when talking about back, shoulder or neck pain even though we have a shit ton of studies that compare the postures of pain free people with those with back, shoulder or neck pain and find no real differences, this information gets regularly IGNORED.
NEVER let science get in the way of a good story, especially if it’s on the interwebs!
In fact I have written about posture a few times before : )
The definitive guide to posture and pain 3 minutes flat
Do you really need your joints to be centred?
But just to kick off with a bit of science, this paper HERE from 2016 found NO significant difference in lumbar lordosis (spinal curve) between people with back pain and those without.
This is super important. HOW can we blame something that we see in people WITHOUT pain as a cause of pain for those that do?
I will just let that sink in……
What are you measuring?
So in this blog we are going to explore a few questions related to how we assess posture and if they are actually scientifically VALID, because if you don't have a good measure to begin with then it is pretty tough to blame something for the problem.
The first piece of ACTUAL EVIDENCE, something often missing in the posture debate, looks at the measurement of STANDING LUMBAR LORDOSIS (the curve in the back often blamed for back pain) and this assessment is something that is performed in treatment rooms and gyms the world over.
The idea is that an increase (and sometimes decrease) in lumbar curve increases back pain and is often coupled with the idea that the tilt of the pelvis has an influence on the size of the lumbar curve, even though lumbar curves do not seem to be much of a factor in lower back pain anyway (see the SCIENCE above : )
Way back in 1990 this was explored by Heino et al HERE and they found that the angle of someones pelvic tilt and their lumbar curve do not simply correlate! So looking at the position of the pelvis tells us very little about what is occurring at the lumbar spine, which is much harder to measure. A very similar study HERE from before this in 1987 also threw up the same result but this BS is still being taught today.
Anyway, back to the standing measurement paper HERE. The authors explored the variability in standing posture of 400 people, 332 without pain and 83 with low back pain, and they found that each time we stand we do it in a slightly different way.
The authors in their words state “standing is highly individual and poorly reproducible”.
So why does this matter?
Well simply put, which posture are you ACTUALLY measuring with your postural assessment. One may show an increase in lordosis, another less so.
I have some questions related to how we interpret postural assessments in light of this information.
- Which of these postures is related to the problem?
- How many times do you measure and do you average?
- What are you comparing against to determine if the curve is too much or not enough?
The authors highlight a good point that the lack of consistency in standing posture may actually lead to the “wrong diagnosis and possibly unnecessary treatment”.
If you focus on something that is not an issue you do not focus on something else that might be or be blinded to the fact that it is not working or only works transiently (potentially why so much back pain is persistent).
What people actually use in their everyday lives might also be different to what is measured in the clinic or gym. A clinic or gym measure could be described as a ‘snapshot’ and this study HERE compared this ‘snapshot’ to what was actually used on a daily basis by the study participants.
The authors found that on average whilst standing, as most postural assessments are, there was a 33.3° lumbar lordosis but the average used over a 24hr period was only 8°, a huge difference!
So the ‘snapshot’ postural assessment would not really inform us very well about how much lordosis was REALLY being used and we could overestimate the extent of the imaginary problem : )
We also have to remember these were radiological measurements and this is the clinical ‘gold standard’. Often a lordosis is measured in a much more rudimentary fashion by looking at the relationship of landmarks at the pelvis indicating a pelvic tilt and therefore change in lumbar curve, which we have already discussed as not being well related to lumbar curve! This in itself is a problem as demonstrated by Preece in 2008 HERE as pelvic morphology is also VARIABLE leading to incorrect measures.
“These results suggest that variations in pelvic morphology may significantly influence measures of pelvic tilt and innominate rotational asymmetry”
Here is the distribution of side to side difference of the ASIS-PSIS relationship (used to assess pelvic tilt), we can see it is skewed to the right side meaning it is more anteriorly tilted at a BONY level.

So it might be that we are really bad at measuring something that doesn’t matter that much. OUCH
Are you biased?
Another important question for those that assess posture is……are you MORE inclined to see an ‘abnormality’ in posture when you know pain is present?
This paper HERE would suggest so Here the authors looked at scapular dyskinesis or abnormal posture and movement of the shoulder blade, which is often proposed as a CAUSE of shoulder pain.
They compared 67 people with shoulder pain and 68 without and firstly found that there was no difference in shoulder posture or motion between those with pain and those without.
Fascinatingly though when the assessors were aware that they were assessing someone IN PAIN, they reported a greater prevalence of a postural or movement problem. This shows a bias towards to finding an ‘abnormality’ to blame when there is pain, even though there was NO MORE ‘abnormality’ in those with pain than without.
The authors also suggest that scapular dyskinesis actually represents normal variability between humans! Perhaps if they assessed it multiple times it would throw up different measures each time?! It is important to remember we have no scientifically defined ‘good posture’ to base deviations from in the first place.
How do healthy people sit?
Another question is how do people without back pain actually behave? They must have great daily posture right? Well actually NO.
This paper HERE shows that asymptomatic folk , 50 of them, when seating actually SLUMP. In 10-min sitting, spinal angles flexed 24 deg at lumbar and 12 deg at thoracolumbar regions relative to standing posture. But this slumping does not seem to cause them problems.
So changes in our spinal curves seem to be fairly unrelated to pain as we can see below.

So if posture does not really correlate with pain, what does it correlate with?
Well this paper HERE shows that cervical spine alignment changes actually correlate with age. This study split the participants into 4 groups determined by age. They found that the measures of the angles of the neck all correlated with the increasing age range of the 4 groups.
Key point to remember here is that all the participants, 120 of them, had no pain. In fact the exclusion criteria here was pretty rigorous and the authors actually excluded 64 people, so 1/3 of the original sample, for having current or previous pain.
So simply put, as we get older our posture becomes ‘worse’ or perhaps better put our posture increases....BUT and a this a big BUT, this does not seem to cause MORE pain.
To sum up it does not seem as simple as ‘bad’ posture = pain whatever you read or are told in a bar, gym or clinic room.
Key take homes
- People IN pain DON’T have different postures to those that don’t have pain
- Posture displays variability just like movement
- This means your assessment may not tell you what you think it does
- Your assessment could be biased to finding a postural ‘problem’
- Postures used throughout the day are probably different to those being assessed
- As we get older our posture change and this happens to people NOT in pain too
Here is a FB live lecture on adherence with lots of research discussed around this topic and a sprinkling of opinion too!
Here are the slides too! Adherence (1)
So I got my virtual buddy Paul Lagerman AKA the naked physio to come in and contribute to this post and below is our bastard lovechild offspring of a blog post : )
The video above on whales and their contribution to our planet is not only informative and enlightening but also serves as a great metaphor for our understanding of the human body.
Confused? Read on.
An argument for the continuation of whale hunting is that whales are predators that sit at the top of the food chain and consume fish. One school of thought would be if we reduce the number of predators then there will be more fish for the smart Humans to eat. Sounds simple right?
Well, actually….not so much!
The video nicely highlights the complex interaction between the whales and other inhabitants of the sea such as fish, krill and plankton. In fact what has been found is that as we reduce the number of whales so has the number of fish reduced, disturbing the homeostatic balance of the ecosystem. Interestingly, causation is not a simple correlation of reducing numbers of one thing will increase the numbers of the other.
Why?
Well as usual what seems like a simple relationship turns out to not be so simple, and the reasoning model used to come to this conclusion is well….. simply wrong.
Surprise surprise.
The whales as it turns out have a much more complex interaction with the environment so there are things that have simply NOT been considered in the simplistic model.
The whales actually bring nutrients up to the surface in the form of whale poo that are much scarcer in the upper waters and in turn help to fertilise plant plankton. They also create changes in the vertical water flow by moving up and down the water column that also has an effect on the plank plankton and enables them to thrive.
The animal plankton feed on the plant plankton that in turn feeds the smaller fish and krill and so the food chain flourishes, it moves and it flows.
So simply put more whales equals MORE fish and krill, not LESS.
Thinking about the impact of just one system in the biological world where more than one system interacts is just well plain STUPID even if it is simple and makes sense to some people. The aquatic ecosystem is multidimensional, approaching it with a unidimensional reasoning model will always have trade offs.
Remind you of another model?

The parallels with the human body are quite stark. The body is a complex system made up of many systems that interact such as the mechanical, biological and psychological. We can break it down further into the cardio vascular, muscular endocrine etc etc and all of these systems interact. The body depends on a homeostatic balance and interaction between systems similar to that of the aquatic ecosystem.
When we view the body simply as a mechanical system operating in a linear fashion, it makes complete sense that if we keep moving in a specific or repetitive way we will produce increase stress to muscles and bones that eventually will fail and cause pain, or that the knock on effect of excessive or decrease movement will cause a problem somewhere else.
Is this a bit like thinking less whales equals more fish?
Well here’s the problem, maybe we have applied the wrong model that does not consider other factors involved with being a human just like the whale guys.
Firstly, human beings are not simply a mechanical system, they are a biological system that displays both variance and adaptability.
This means that one part does not have a simple knock on effect to another. The body DOES display interdependence but also independence and it does this in a very individual way that simple all encompassing models do not really reflect.
- Humans are adaptable. If we load the body in a variety of dimensions (physical, psychological, social, environmental) it has the ability to get stronger and adapt rather than just wear out like a piece of metal would. How do we know this? Going to the gym and weight training is a great example, or exposing yourself gradually to stimuli such as temperature or a bed of nails.
- It has redundancy and variability. This simply means the body has a whole bunch of ways of achieving the same task that can reduce repetitive loads that might have a detrimental effect. This is a key defining feature of a biological system.
- The human body has individual tolerances. Some people can compete in iron men triathlons whilst others struggle to run 5K. Just because you apply a load to a tissue does not mean it will be beyond its tolerance, especially if it has successfully adapted to the load.
We also have to consider the impact on other co existing systems such as the psychological or social.
If you tell a person moving is bad then they may form a belief that moving is bad and stop moving, or perhaps your workplace has specific rules about lifting technique and this influences the way you protect your back. We are very impressionable creatures after all.
Stopping people from flexing their spines is a great example of a simple mechanical view having an effect on the psychosocial perception of movement or activity and a potential detrimental outcome.
If I do not flex my spine due to the belief that this is BAD, its tolerance to moving and flexing might actually DECREASE as it is not being loaded. Astronauts do not load their bodies as much due to decreased gravity. Their bodies and bone mass adapt negatively, a process of atrophy (remember adaptation happens both ways). This can also happen after immobilisation of a limb following a fracture or a sprain, consider the long term effects of complex regional pain syndrome.
So in essence one system, the psychological or social has had an effect on another system - the biological, all of this originating from a mechanical viewpoint. A familiar image of categorical thinking and reductionism is depicted in this image.

So even though things seem simple and make sense, consider that simple may not always explain the cause.
Be more WHALE and less HUMAN.
Here is the link for the Facebook live lecture on back pain.
Here is a link to download all the slides in a PDF format too!
FB Back Pain (1)
Here is a fantastic guest blog from Luke R Davies on Listening as therapy, Louis Gifford's ABCDEFW framework & yellow and pink flags concept.
Luke is really into movement, pain and most of all helping his patients recover with a fun and active approach to rehab and probably why we get on so well!
Enjoy!

Listening is a significant part of the therapeutic encounter, we have to work on it.
Louis Gifford (2014)1 first put forward the mnemonic ABCDEFW as a framework to guide the clinician through important questioning regarding psychosocial risk factors.
Once red flags have been ruled out and the predominant pain type established, a distinction between adaptive and maladaptive pain can be made. Adaptive pain is beneficial to the organism and alerting to perceived threat whereas in maladaptive pain the issue is in the nervous system itself, an analogy being the 'pain' alarm has been sensitised.
Diener et al. (2016) 2 describe how psychosocial factors are often attributable to a sensitised nervous system, also known as 'yellow flags'. It can be suggested that in any case where pain has persisted beyond the expected healing times of the tissue involved that there is some element of sensitisation (Louw & Puentedura, 2013). 3Almost all tissues in the body heal within 3-6 months (Louw, 2014) 4.

Pyschosocial factors are referred to in the literature as yellow flags
Yellow flags have been shown to predict worse outcomes in clinical practice. While there remains debate within the field, it has been shown that targeting these factors as part of the intervention does improve clinical outcomes (Nicholas et al. 2011)5.
The mnemonic ABCDEFW enables the clinician to explore those factors that need challenging and potentially reconceptualising. An expansion of the mnemonic was produced by Diener et al. (2016)2 in a great paper aptly titled 'listening is therapy':
ATTITUDES & BELIEFS
Key Question: What do you think is the cause of your pain?
Information gained:
- Fear avoidance
- Catastrophization
- Maladaptive beliefs
- Passive attitudes toward rehabilitation
- Expectations of effect of activity or work on pain
BEHAVIOURS
Key Question: What are you doing to relieve your pain?
Information gained:
- Use of extended rest
- Reduced activity levels
- Withdrawal from activities of daily living (ADL) and social activities
- Poor sleep
- Boom-bust behaviour
- Self medication - alcohol, over the counter (OTC) or other substances
COMPENSATION ISSUES
Key Question: Is your pain placing you in financial difficulties?
Information gained:
- Lack of incentive to return to work
- Disputes of eligibility for benefits, delay in income assistance
- History of previous claims
- History of previous pain and time off work
DIAGNOSIS & TREATMENT
Key Question: You have been seen and examined for your pain? Are you worried that anything may have been missed?
Information gained:
- Health professional sanctioning disability
- Conflicting diagnoses
- Diagnostic language leading to catastrophization and fear
- Expectation of 'fix'
- Advice to withdrawal from activity and/or job
- Dramatisation of back pain by health professional producing dependency on passive treatments
EMOTIONS
Key Question: Is there anything that is upsetting or worrying you about the pain at this moment?
Information gained:
- Fear
- Depression
- Irritability
- Anxiety
- Stress
- Social anxiety
- Feeling useless or not needed
FAMILY
Key Question: How does your family react to your pain?
Information gained:
- Over protective partner / spouse
- Solicitous behaviour from spouse
- Socially punitive responses from spouse
- Support from family for return to work
- Lack of support person to talk to
WORK
Key Question: How is your ability to work affected by your pain?
Information gained:
- History of manual work
- Job dissatisfaction
- Belief work is harmful
- Unsupportive or unhappy current work environment
- Low educational background
- Low social-economic status
- Heavy physical demands of work
- Poor workplace management of pain issues
- Lack of interest from employer
Louis Gifford describes how targeting these factors identified through ABCDEFW questioning can turn otherwise indicators of a poor outcome into indicators of a good one. These have been described as 'pink flags'.
EXAMPLE
If someone with persistent pain has become dependent on passive coping strategies (bed rest, clinician 'fixing' them through passive techniques like manipulation or needling, amongst many others...) this is a yellow flag.
If these beliefs have been successfully challenged and reconceptualized then this person would move towards a much more proactive approach to managing not only their pain, but them-selves. This is a significant factor in predicting better outcomes in terms of disability5 and serves as an example of a 'yellow flag' turning into a 'pink flag'.
Listening is therapy, make sure you can guide the interaction with appropriate questioning (ABCDEFW) so as what you listen to can actually influence outcomes for the better.
Luke R. Davies :)
REFERENCES
1. Gifford, L. (2014). Aches and Pains: TJ International, Padstow, Cornwall, UK.
3. Louw, A. and Puentedura, E. (2013). Therapeutic Neuroscience Education; Teaching Patients About Pain, International Spine and Pain Institute, USA.
4. Louw, A. (2014). Why You Hurt, Neuroscience Pain Education Cards, International Spine and Pain Institute.
5. Nicholas, M., Linton, S. J., Watson, P. J. and Main, C. J. (2011). Early identification and Management of Psychological Risk Factors ("Yellow Flags") in Patients with Low Back Pain: A Reappraisal, Working group. Physical Therapy; Washington, P.737-53.
In all honesty in its current format the answer here has to be an unreserved YES, we should STOP assessing movement.
This opinion is based on the two predominant concepts we appear to have currently when assessing movement.
Firstly the concept that a deviation from a movement or muscle firing ‘ideal’ is the cause of someone’s pain such as seen with the pathokinesiology model.
Secondly that we can also ‘screen’ movement to identify faulty movement that might lead to injury, this is FAR too big a subject to get into but it seems we weekly have new data suggesting screening does not fulfil the role it was designed for.
Both of these concepts have so far proved to be elusive in providing concrete evidence that they do exactly what they say they do.
A modern understanding of all the contributors to pain means the likelihood of pain being consistently caused by one single factor across ALL people is pretty absurd really.
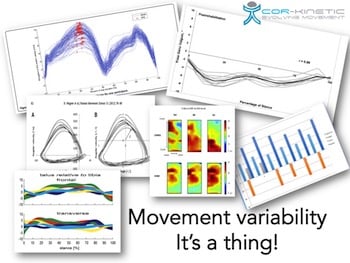
It's VARIABLE
The more we study movement the more we find that it is in essence highly variable. This variability is not only between people but even the same person seems to move differently when they repeat a movement. It has been suggested, and with a fair amount of evidence, that healthy movement is variable and losing variability maybe a problem within itself. It is important to realise this about movement because it allows us to appraise the idea of movement assessment more critically.
I have previously discussed this *Here* and *Here* along with the concept of corrective exercise.
Now this means that being able to identify a ‘faulty’ movement pattern will be highly likely if you are measuring it against a singular ‘ideal’ version. The problem is the singular ideal version does not really exist and also does not seem to be linked to very much, rendering the whole process a bit of a waste of time.
It makes little sense not to be variable:
- Multiple options affords us redundancy
- Ability to respond to varying stimulus
- Spreading load over a joint in repetitive tasks
- Avoiding fatigue through variable motor unit recruitment
- Unavoidable at a biological level
We also may go further down the rabbit hole in that some now ASSUME that pain is simply the RESULT of a faulty movement pattern without any kind of critical analysis at all. Think how some people approach back pain, "Its your TvA not be firing" rather than lets find out if it is or not (obviously no clinical test tells us this, just an example).
Movement does not equal force
Now I am no biomechanist but we also must realise that just because a movement goes into a potentially ‘faulty’ position does not tell us the whole picture of how much damage that poses to a tissue. Sure it might increase the risk in some contexts but alone it does not give you the ACTUAL force applied and we would also need to know the acceleration as well. A fast movement within proposed ‘safe’ parameters that generates a large force (F=MA) could provide a much greater load to a tissue than one that was proposed as ‘faulty’ that moved much slower.
In fact under greater loads our movement seems to change, so assessing in a low load environment may not give you an indication of how movement is in another situation. This was an interesting piece from Frost et al *Here* showing exactly that!
Some seem to have developed the idea that if you get a movement right you can put it under ANY load. The way the body manages loads internally through the way it moves may be far LESS important the overall volume of load that the body may go through overall and this could be in volume, frequency or intensity.
A different perspective?
So can we STILL look at movement in practice, I believe so. Everything has it uses and limitations and its working out WHEN thats the tough bit.
Pain DOES have an effect on the way we move, this is pretty well researched showing alterations in what happens with both kinematics AND kinetics at a joint, to adjacent joints and right up to avoiding movement completely for fear of pain. This is a great paper by Hodges & Smeets discussing this *HERE*
Like any other thing that we can measure, it may or may not be related to the problem and may or may not have to change to get a successful result.
Certainly it very difficult to suggest that the way someone moves is a cause of their problems. Do you know what it looked like before? Could it be the RESULT not the cause or pain? BUT is there also a possibility that a change in movement strategy COULD also have an effect on reoccurrence or another injury. We know that the best predictor of future injury is previous injury *Here* and this could be a factor. This has also been mooted with back pain *Here*.
It is a good place to use your reasoning skills. Is this the first time it has happened? Is it acute? Both of these simple questions might help to determine if it is currently an adaptive strategy (helpful) because of pain or is it a maladaptive behaviour (unhelpful) that maybe contributing to the maintenance or reoccurrence of a problem.
Look at the INDIVIDUAL
A potentially more individualised concept for how we view movement is that rather than a binary right and wrong view that we have currently, we could say your current strategy is unhelpful and swapping that for another might be more helpful, there are often a whole bunch of other ways that could be beneficial rather than the 'right' way.
This might only be for the short term, such as a symptom modification, or for the longer term if you believe a movement behaviour maybe coupled with a pain response.
Gait re-eduction for runners seems to follow this rationale, see whats going on, does that potentially relate to the issue and can we subtly alter it.
Now there maybe certain scenarios that do carry more risk such as loaded lumbar flexion or extreme knee valgus but they seem to be pretty load related. Unless someone is regularly under these loads perhaps it matters less. But ask yourself how many people in the gym have popped an ACL doing a single leg squat? Perhaps the caution can cause more problems than it solves here? Especially with the unhelpful beliefs people seem to be prone to forming.
Some examples of unhelpful
It could be that a movement loads a specific body part that is currently sensitive
Example
If some one has a very hip driven strategy whilst currently suffering from a proximal hamstring tendinopathy altering this could reduce further load/compression to the tendon to allow it to desensitise.
Pre movement behaviours
It could be that be that someone is bracing BEFORE they move and this is an unhelpful component. This maybe seen with lower back pain sufferers.
Example
Before bending over to do their shoelaces someone specifically braces and this has become coupled with the pain they are experiencing. Attempting to change this part of the motor strategy MAY affect the outcome.
It could be they only have ONE movement strategy
We see decreased variation linked with chronic pain at a number of areas of the body. This could cause repetitive loading or consistent patterns ASSOCIATED with pain.
Example
A specific task maybe is performed in a repetitive way. This might be the way someone lifts, reaches or even runs. A way to assess this could be to provide variable challenges and see how well someone can adapt.
What we do have to remember that this is all TRIAL & ERROR.
It may or MAY NOT have an effect and essentially this is everything we do. We should try to be informed by current best evidence but also remember is just a probability generated in a controlled environment and may not directly translate to this person you are dealing with.
Take aways
- Specific movement ideals are pretty unsupported, especially linking them to pain
- Movement screening is literally a can of worms
- Movement is variable, EMBRACE it! This means it is tough to assume causative link with pain
- Low load assessment tells little about high load behaviour
- A movement does not simple equal the force applied to the tissue
- Look at the individual
- Be prepared that altering movement may have NO EFFECT or a very positive one
We could definitely have a good, and potentially lively, discussion over what makes a great rehab program and with no gold standard here, we will have to settle for some well reasoned opinion.
This being my blog………here is mine!
Exercise & movement are not golden bullets to a successful recovery, far from it, but they do show promising results and can be done BY someone rather than being done TO someone, which is a real positive for behaviour change and on-going self-management.
Commonly when we discuss what makes up the BEST rehab program it will be about promoting some specific type of training or a magic exercise with the highest activation or program design process that gives the best results across ALL people, but perhaps we need to start to think about how we can help just that one person currently in front of us. We also often talk a bit more about the exercises themselves rather than the rehab process.
As always the most powerful exercise available to us is the REASONING process behind the program. I would also add how we then FRAME and EXPLAIN it is pretty important too.
This a reasoning model I made recently that firsts asks the question of what is the outcome you want to get from your rehab? This idea of the desired outcome then influences what we do and how we do it.

Does all this thinking make things more complex? Perhaps a touch. But just because something is simple does not automatically make it more effective. Simple is also not a well-defined term, one persons simple maybe another’s complex and visa versa.
We often are still seduced by seemingly easy answers that are purported to work for everybody and this is a great quote from Don Marquis that sums it up nicely.
“If you make people think they're thinking, they'll love you; But if you really make them think, they'll hate you.”
Anyway, enough philosophising, what does make a good rehab program?
Rather than think in the finer details of program design perhaps we should think in broader brush strokes. Why? Well so far we don’t have much good information on exactly WHAT is the best type of exercise for many painful complaints or exactly how they help.
Rotator cuff tendinopathy HERE
Tendinopathy HERE
Lower back pain HERE
PFP HERE
Achilles tendinopathy HERE
Osteoarthritis HERE
Back pain (again) HERE
Perhaps we could say that doing SOMETHING seems superior to doing NOTHING so finding out some of the things that influence people actually doing their rehab is beneficial.
TIME
A very basic reason that exercises don’t even get performed in the first place, a prerequisite for any training effect, is that they don’t fit in with people’s lives and the time they take to perform. People are time poor with work pressures and family and social pressures and these stressors may even be a contributor to the problem in the first place.
This paper found time to be the number one predictive factor to adherence for a home exercise program HERE.
A rehab plan that does not take into account the doability factor (yes I made that word up) could even ADD to the stress someone is experiencing beyond the fact that it is simply not getting done and is an exercise in futility (get it!). A 12 exercise program requiring specific equipment that is only available a 20 minute drive from the house and requires spending an hour doing them fails miserably when we look at the doability (there it is again) factor.
Simple might be (opinion alert) a small number of exercises that can be easily performed with minimal equipment at a convenient location and time of the day. Rather than it being a specific we can fill in the blanks by interacting with the person who actually has to do it. Although of course as SIMPLE is very subjective it could also be a shit ton of other stuff too! Essentially it is the recipient, the patient, who must define simplicity.
Maybe the actual EXERCISE itself is less important? If there are a whole bunch of ways to skin a cat then we can make the process easier by not being too attached to any single type of exercise.

Perception
Someone’s perception of the program is also important. Perception or expectation of success will drive…..wait for it…..the success of the program. This has been well documented HERE & HERE.
If you don’t believe something will work why would you invest the time and effort in it? So even if the primary mechanism of action of a rehab program is a physical/biological one it may be limited by a belief structure.
This paper here HERE found that the benefit gained from exercise might be mediated by the predicted expectation of the benefit. We have to appreciate that OUR perceived benefit of a specific type of activity may not match the PERSONS. As it their beliefs that mediate the outcome this matters a fair bit.
Previous experiences influence our expectations that in turn may drive future outcomes. If I have previously failed using a specific exercise then this may affect my expectations of something similar having success in the future. This could be by reducing the perceived benefit AND also the effort put into it at a physical level.
So finding out about expectations, taking them in to account when designing a rehab program and potentially addressing them with explanations about WHY certain elements maybe beneficial could have a dramatic effect on the outcome with certain people. The way the exercise is FRAMED maybe as important as the exercise itself.
Exercises that fit in with previous successes or are enjoyable might drive an increased perception of benefit and adherence. How do we find this out? Well this is where we get super simple, just ASK, what activities do you enjoy? Have things worked for this problem in the past? What things haven’t worked?
Imagine someone has failed with rehab after being given a sheet of exercises, would it be best practice to just give them another sheet of exercise?
We could dig a little deeper to find out why did they previously fail?
Did they do the exercises?
If not, why not?
What was their perception of them?
What may need to improve is the ACTUAL use of this information to improve rehab programs.
Don’t forget ACTIVITY
Activity can be a really useful tool as well as more specific targeted exercises and those with long-term pain issues often find that their activity levels can drop and this could contribute to how they feel both physically and psychologically. This could be thing’s that are loved and cherished such as dancing or playing with their kids or activities around the house that need to get done on a regular basis.
People can simply rule out activities because they have previously hurt. This does not mean that they are automatically bad but can be perceived that way. Restarting or maintain activities does not have to have a binary yes or no answer, instead they can be graded and we can attempt to find a tolerable dose.
This paper from Darlow HERE looked at beliefs around back pain with some interesting results.
- 59% believe if an activity causes pain it should be avoided in the future
- 55% believe exercise risk outweighs the benefit
These are some of the perceptions and beliefs that may have to be overcome about activities, especially pain provoking ones, before you even get to the business of moving.
Which activities did they previously do, especially enjoyable ones?
Why don’t they do them anymore?
Did someone suggest they should stop?
Can you find a tolerable dosage and maintain activity or slowly build up?
Advice and On-going support
Advice about the actual process might have a huge influence on the outcome and could make the exercises a whole lot more effective.
- You actually HAVE to do the exercises for them to work (no shit)
- Sometimes put in real EFFORT
- They may take time to work
- They may make you sore - Maybe explain what this means
- Rehab has ups & downs
- If you are stressed and/or time poor do a bit less
- If you are time rich and/or feeling good do a bit more
Another key part of a rehab program is offering on-going support. Ever started to build a piece of flat back furniture and found that the instructions were just to difficult to follow or were incomplete? Who can you call to help? Often nobody. How many pieces of furniture still remain uncompleted? I bet a whole bunch. Probably about as many as we have rehab plans that have not been completed!
Making sure someone is aware that they can access on-going support could make a difference here, even just the knowledge they CAN access some.
Summing up
- We don’t know what type of exercise is BEST for painful complaints
- The one that get’s done probably is the BEST
- That maybe individually defined
- Time matters
- Perception matters
- Activity matters
- Advice matters
- Support matters
Latest Articles
 If 9 out of 10 interventions are a load of rubbish, what the hell do I DO?August 4, 2022 - 3:29 pm
If 9 out of 10 interventions are a load of rubbish, what the hell do I DO?August 4, 2022 - 3:29 pm Why the advice to “rest” & “remain active” can both be a bit rubbish!December 21, 2021 - 2:38 pm
Why the advice to “rest” & “remain active” can both be a bit rubbish!December 21, 2021 - 2:38 pm Why I HATE discussions about treatment…….June 22, 2021 - 6:58 am
Why I HATE discussions about treatment…….June 22, 2021 - 6:58 am Evidence based practice – Do you love or loathe it?March 29, 2021 - 3:09 pm
Evidence based practice – Do you love or loathe it?March 29, 2021 - 3:09 pm- The myth of exercise prescriptions – It’s probably more trial and error than we care to admitOctober 15, 2020 - 11:43 am
 Education in rehab – WTF does it mean…..?October 1, 2020 - 12:15 pm
Education in rehab – WTF does it mean…..?October 1, 2020 - 12:15 pm
SIGN UP FOR UPDATES

